The interplay between genetics and gastrointestinal diseases is a fascinating and complex area of study that sheds light on the inherited factors contributing to the development of various conditions affecting the digestive system.
Our genetic makeup is a deciding factor in influencing susceptibility, severity, and progression of gastrointestinal disorders. Understanding these genetic predispositions is crucial for both identifying individuals at higher risk and devising targeted therapeutic interventions.
Genetic predispositions to gastrointestinal diseases often involve a combination of inherited genetic variants and environmental factors. Specific genes may influence how our digestive system functions, impacting processes such as immune response, inflammation regulation, and the maintenance of the gut barrier.
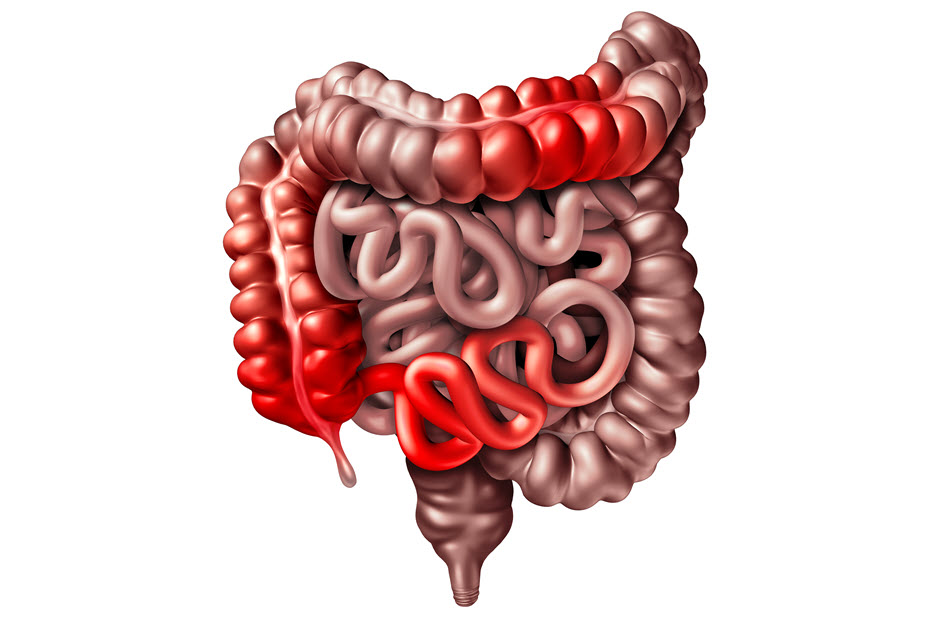
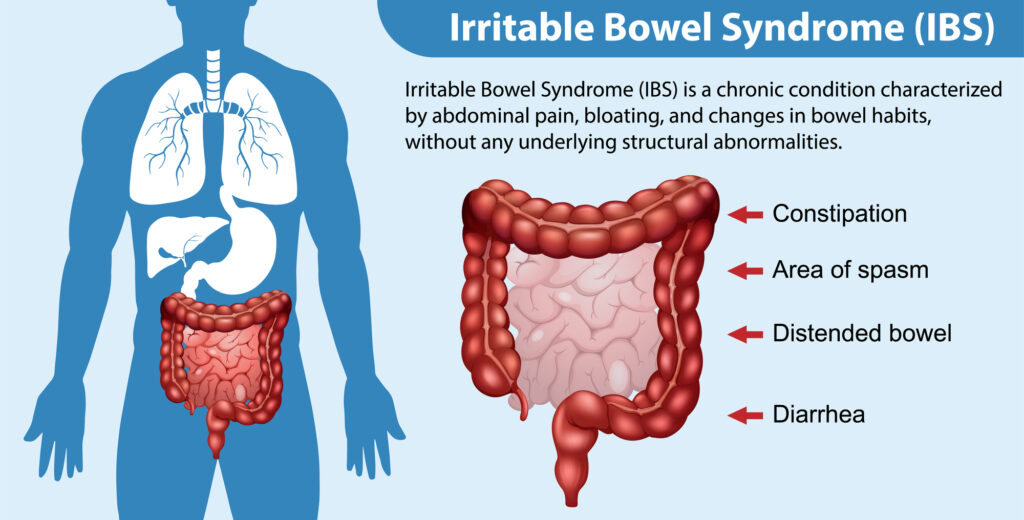
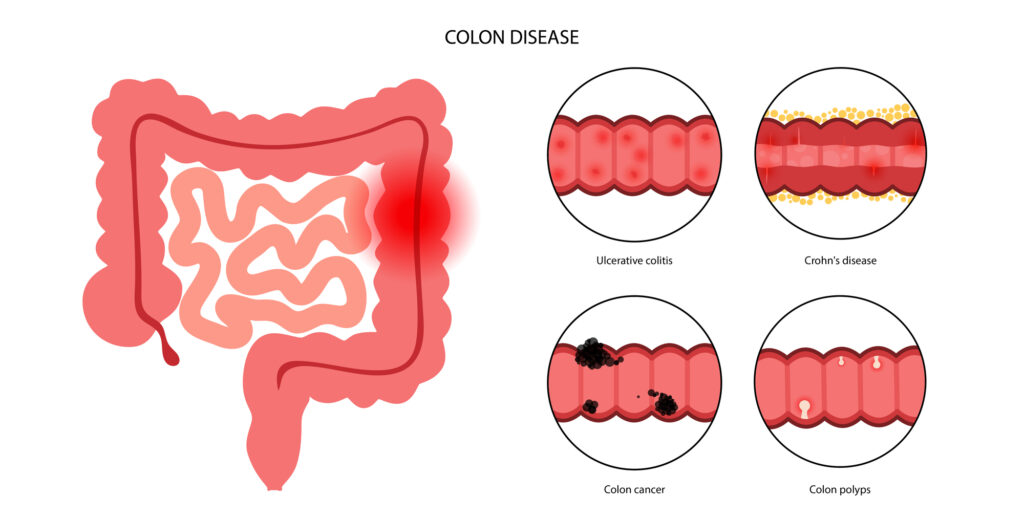
In conditions like inflammatory bowel disease (IBD), genetic factors contribute significantly to an individual’s susceptibility. Variants in genes associated with the immune system, such as those related to the interleukin family, have been implicated in increasing the risk of developing Crohn’s disease or ulcerative colitis.
In other instances, genetic mutations can affect the metabolism of specific substances, making individuals more susceptible to conditions like hereditary hemochromatosis, where excess iron absorption can lead to gastrointestinal complications. Conditions like celiac disease have a strong genetic component, with specific human leukocyte antigen (HLA) genes influencing an individual’s predisposition to gluten intolerance.
While genetic predispositions create a foundation for susceptibility, environmental factors such as diet, lifestyle, and exposure to certain triggers also play a crucial role in the manifestation of gastrointestinal diseases.
GI Diseases Influenced by Genetics
In unraveling the genetic basis of these major gastrointestinal diseases, researchers are paving the way for personalized medicine approaches, early interventions, and a deeper understanding of the complex interplay between genetics and environmental factors in maintaining digestive health.
Below are some specific GI diseases that are influenced by genetics.
Inflammatory Bowel Disease (IBD)
Genetic predisposition is involved in the development of IBD, which encompasses both Crohn’s disease and ulcerative colitis. Variants in genes associated with the immune system, such as those involved in the regulation of inflammation, significantly contribute to an individual’s susceptibility.
Gastrointestinal Cancers
Several gastrointestinal cancers, including colorectal, gastric, and pancreatic cancers, have genetic influences. Inherited mutations in specific genes, such as those associated with Lynch syndrome for colorectal cancer or hereditary diffuse gastric cancer syndrome (CDH1 gene) for gastric cancer, can elevate the risk of developing these malignancies.
Celiac Disease
Celiac disease, an autoimmune disorder triggered by gluten consumption, has a strong genetic component. Specific human leukocyte antigen (HLA) genes, particularly HLA-DQ2 and HLA-DQ8, are associated with increased susceptibility. Individuals carrying these genetic markers are more prone to developing celiac disease when exposed to gluten-containing foods.
Lactose Intolerance
Lactose intolerance, characterized by the inability to digest lactose, the sugar found in milk and dairy products, can have a genetic basis. The persistence or decline of lactase activity, the enzyme responsible for lactose digestion, is influenced by genetic variants.
Certain populations, particularly those of East Asian, African, and Native American descent, commonly exhibit a genetic predisposition to lactose intolerance into adulthood, emphasizing the ethnic variability in lactase persistence.
Peptic Ulcer Disease
Finally, while the majority of peptic ulcers are caused by Helicobacter pylori infection, genetic factors also contribute to an individual’s susceptibility. Variants in genes involved in mucosal defense, acid secretion regulation, and inflammatory response can influence the likelihood of developing peptic ulcers.
Treatment, Management, and Prevention
Advances in genetic research have ushered in an era of personalized medicine, offering tailored approaches to treat gastrointestinal diseases influenced by genetics. Targeted therapies aim to address the specific molecular and genetic factors contributing to the disease.
In cases of gastrointestinal cancers with known genetic mutations, such as EGFR in colorectal cancer, targeted therapies can be more effective and less invasive than traditional treatments, leading to improved outcomes and reduced side effects.
Role of Genetics in Treatment Selection and Efficacy
Understanding a patient’s genetic profile is increasingly influencing treatment decisions. In certain conditions like inflammatory bowel disease (IBD), genetic testing can help predict response to specific medications.
For instance, genetic variants in the TPMT gene can impact the metabolism of thiopurine medications, guiding clinicians in adjusting doses to minimize side effects and enhance efficacy.
Dietary Components and Lifestyle
Genetic predispositions can also influence how individuals respond to certain dietary components and lifestyle factors. In conditions like celiac disease, where gluten intolerance is genetically determined, strict adherence to a gluten-free diet is the primary mode of management.
Similarly, understanding one’s genetic predisposition to lactose intolerance may guide dietary choices, with some individuals benefiting from lactose-free or reduced lactose diets.
Recognizing the familial nature of many gastrointestinal diseases and screening individuals with a family history is crucial for early detection and prevention. Regular screenings, such as colonoscopies for those with a family history of colorectal cancer, can aid in identifying precancerous lesions at an early, more treatable stage.
Additionally, genetic counseling can provide valuable insights for individuals with a family history of conditions like hereditary pancreatitis or Lynch syndrome, informing them about potential risks and preventive measures.
Finally, beyond genetic considerations, lifestyle modifications play a vital role in preventing and managing gastrointestinal diseases. Maintaining a balanced and healthy diet, rich in fiber and nutrients, can contribute to digestive health.
Final Thoughts
The integration of genetic insights into the treatment, management, and prevention of gastrointestinal diseases marks a useful transition towards more personalized and effective healthcare.
As our understanding of the genetic basis of these conditions deepens, so too does the potential for targeted interventions that consider the individual’s unique genetic makeup, fostering better outcomes and improved quality of life.


“Если вы ищете полезный [url=https://seoblog360.ru/]seo блог кейсы продвижения[/url], то этот ресурс станет вашим надежным помощником в изучении и применении SEO-стратегий.”
Ниша должна быть востребованной, но не слишком конкурентной. Это позволит быстрее выйти в топ поисковиков. Изучите конкурентов, чтобы определить их слабые места.
Не менее важно учитывать свою экспертность в выбранной области. Если вы разбираетесь в теме, контент будет более качественным.
#### **2. Оптимизация контента под поисковые системы**
SEO-оптимизация — ключевой фактор продвижения блога. Каждая статья должна содержать релевантные ключевые слова. Также важно работать с метатегами. Оптимизированные заголовки увеличивают CTR.
Структура текста тоже играет роль. Короткие предложения и четкие формулировки улучшают восприятие.
#### **3. Продвижение и привлечение трафика**
Без продвижения даже качественный контент останется незамеченным. Используйте соцсети для привлечения первой аудитории.
Еще один эффективный метод — внутренняя перелинковка. Это также помогает равномерно распределять вес между страницами.
#### **4. Монетизация SEO блога**
Когда блог набирает трафик, можно задуматься о заработке. Продажа рекламных мест напрямую выгодна при высокой посещаемости.
Дополнительные возможности включают инфопродукты. Электронные книги и вебинары могут стать стабильным источником дохода.
—
#### **1. Выбор ниши для SEO блога**
Проведите анализ ключевых слов, чтобы понять потенциал ниши.
#### **2. Оптимизация контента под поисковые системы**
Title и Description влияют на кликабельность в выдаче.
#### **3. Продвижение и привлечение трафика**
Это также помогает равномерно распределять вес между страницами.
#### **4. Монетизация SEO блога**
Создайте платные курсы или гайды по своей нише.